Introduction
Biomedical engineers play a critical role in ensuring the safety, accuracy, and reliability of medical imaging and diagnostic equipment. From CT and PET/CT systems to DR, C-ARM, and nuclear medicine equipment, even a small maintenance oversight can lead to downtime, safety risks, or diagnostic errors.
Despite experience and technical knowledge, certain maintenance mistakes biomedical engineers should avoid continue to appear in hospitals and diagnostic centers. These mistakes often lead to repeated breakdowns, poor image quality, regulatory issues, and unnecessary costs.
This blog highlights the top 10 maintenance mistakes biomedical engineers should avoid and explains how proper practices improve equipment reliability, patient safety, and long-term system performance.
1. Skipping Scheduled Preventive Maintenance
One of the most common mistakes is delaying or skipping preventive maintenance because equipment appears to be “working fine.” Imaging systems often degrade silently, and problems surface only when failure is severe.
Skipping preventive maintenance can result in:
- Calibration drift
- Overheating components
- Detector instability
- Sudden system shutdowns
Preventive maintenance is designed to prevent failures, not respond to them.
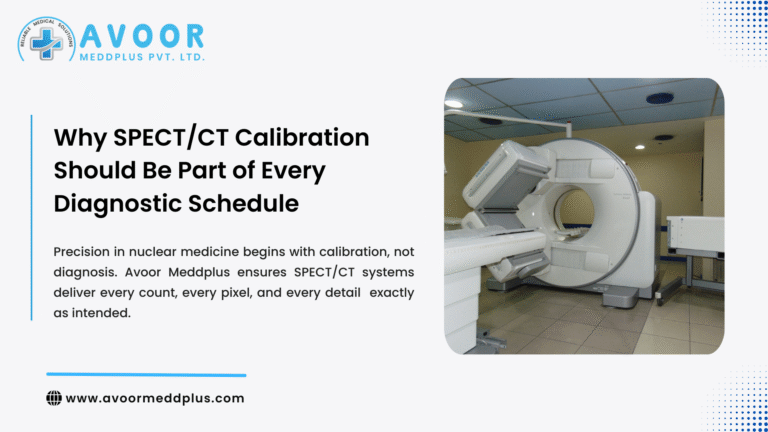
2. Ignoring Calibration Intervals
Calibration is not optional. Many biomedical engineers treat calibration as a corrective task rather than a routine requirement.
Ignoring calibration schedules can cause:
- Inaccurate image output
- Incorrect radiation dose delivery
- PET/CT or SPECT/CT misregistration
- Poor diagnostic confidence
Regular calibration ensures systems operate within OEM specifications and regulatory limits.
3. Relying Only on Breakdown Maintenance
Reactive maintenance increases cost, downtime, and clinical disruption. Waiting for a system to fail before acting is one of the most expensive mistakes biomedical engineers should avoid.
Breakdown-only maintenance leads to:
- Emergency service costs
- Longer downtime
- Unplanned patient rescheduling
- Loss of hospital revenue
A balanced approach combining preventive maintenance and fast corrective response is essential.
4. Inadequate Documentation of Service Activities
Poor or incomplete documentation is a major compliance risk. Biomedical engineers sometimes perform maintenance correctly but fail to record it properly.
Missing documentation can cause:
- NABH or AERB audit issues
- Lack of maintenance history
- Difficulty in root-cause analysis
- Accountability gaps
Every service visit, calibration, and safety check must be documented clearly and consistently.
5. Overlooking Environmental Factors
Many equipment issues are caused by environmental conditions rather than component failure. Biomedical engineers sometimes focus only on internal hardware and ignore surroundings.
Common environmental mistakes include:
- Poor ventilation
- Dust accumulation
- Power fluctuations
- Inadequate grounding
- High humidity
Controlling the environment is critical for long-term equipment stability.
6. Using Non-Approved or Low-Quality Spare Parts
Cost pressure often leads to the use of non-OEM or incompatible spare parts. This is a high-risk maintenance mistake.
Poor-quality parts can cause:
- Repeated failures
- Safety risks
- Signal instability
- Warranty or compliance issues
Using OEM-approved or certified equivalents ensures reliability and safety.
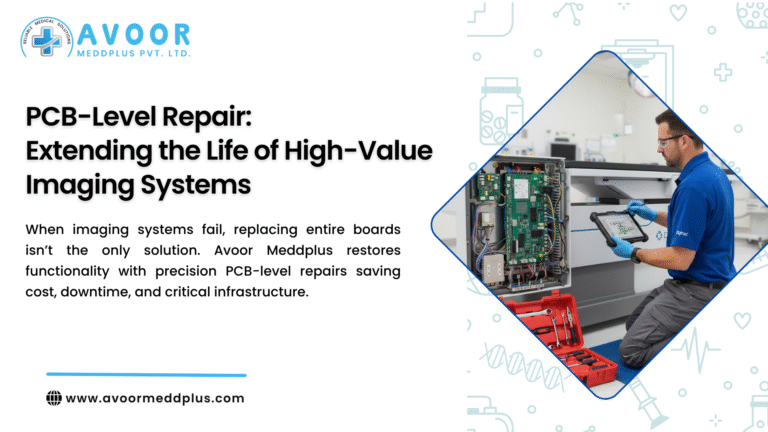
7. Neglecting PCB-Level Fault Diagnosis
Replacing complete boards without analyzing PCB-level issues is both costly and inefficient. Many failures originate from small components such as capacitors, connectors, or ICs.
Ignoring PCB-level diagnostics leads to:
- Unnecessary board replacement
- Higher maintenance costs
- Repeat failures
Biomedical engineers should prioritize component-level troubleshooting whenever possible.
8. Delaying Response to Minor Errors and Alerts
Minor warnings, error logs, or intermittent issues are often ignored until they become critical failures.
Early signs include:
- Occasional system freezes
- Minor image artifacts
- Temperature warnings
- Communication errors
Prompt attention to early alerts prevents major breakdowns and extended downtime.
9. Lack of Cross-Modality Knowledge
Modern hospitals operate multiple imaging modalities. Biomedical engineers sometimes specialize too narrowly and struggle with multi-modality environments.
This leads to:
- Delayed troubleshooting
- Dependency on external vendors
- Inconsistent maintenance quality
Continuous training across CT, DR, C-ARM, PET/CT, and nuclear medicine systems is essential.
10. Poor Coordination With Clinical Teams
Maintenance is not only a technical task; it also involves coordination with radiologists, technicians, and OT staff.
Poor communication can cause:
- Improper scheduling
- Incomplete functional testing
- Workflow disruption
Biomedical engineers should align maintenance activities with clinical operations to ensure smooth service execution.
Why Avoiding These Maintenance Mistakes Matters
Avoiding these maintenance mistakes biomedical engineers should avoid delivers measurable benefits:
- Higher equipment uptime
- Better diagnostic accuracy
- Improved patient safety
- Lower long-term maintenance costs
- Audit-ready compliance
- Stronger trust from clinical teams
Consistent best practices separate reactive maintenance from professional biomedical engineering.
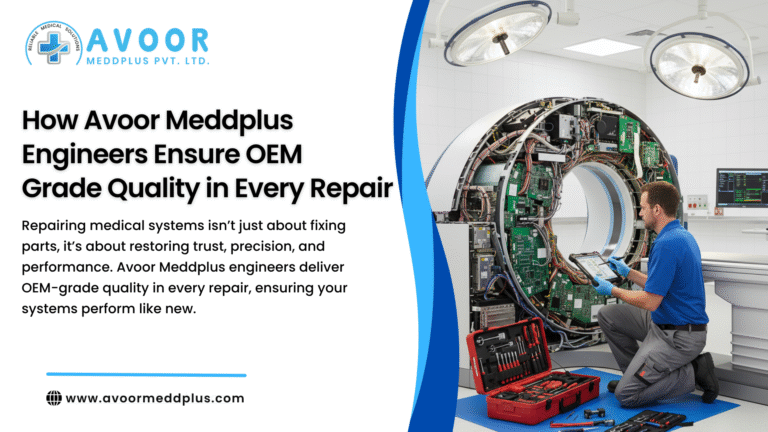
How Professional Service Partners Support Biomedical Engineers
Experienced service partners support biomedical engineers by providing:
- Structured preventive maintenance
- OEM-grade calibration
- PCB-level repair expertise
- Fast response during breakdowns
- Detailed service documentation
- Regulatory compliance support
This collaboration helps biomedical teams focus on performance, safety, and reliability.
Conclusion
Maintenance excellence is built on discipline, awareness, and proactive action. The top 10 maintenance mistakes biomedical engineers should avoid highlighted in this blog are often responsible for avoidable downtime, safety risks, and diagnostic errors.
By following preventive schedules, respecting calibration protocols, maintaining documentation, and responding early to issues, biomedical engineers can significantly improve equipment performance and clinical reliability.
Strong maintenance practices protect not only machines—but patients, workflows, and institutional reputation.